Pigmentation disorders are among the most common concerns in dermatology and aesthetic practice. While often perceived as a cosmetic issue, pigmentation reflects complex interactions between melanocytes, keratinocytes, inflammation, hormones, and environmental triggers. Effective management begins with accurate diagnosis, understanding depth and aetiology, and selecting appropriate in-clinic modalities rather than relying on topical therapy alone.
Melanin Biology: The Foundation of Pigmentation
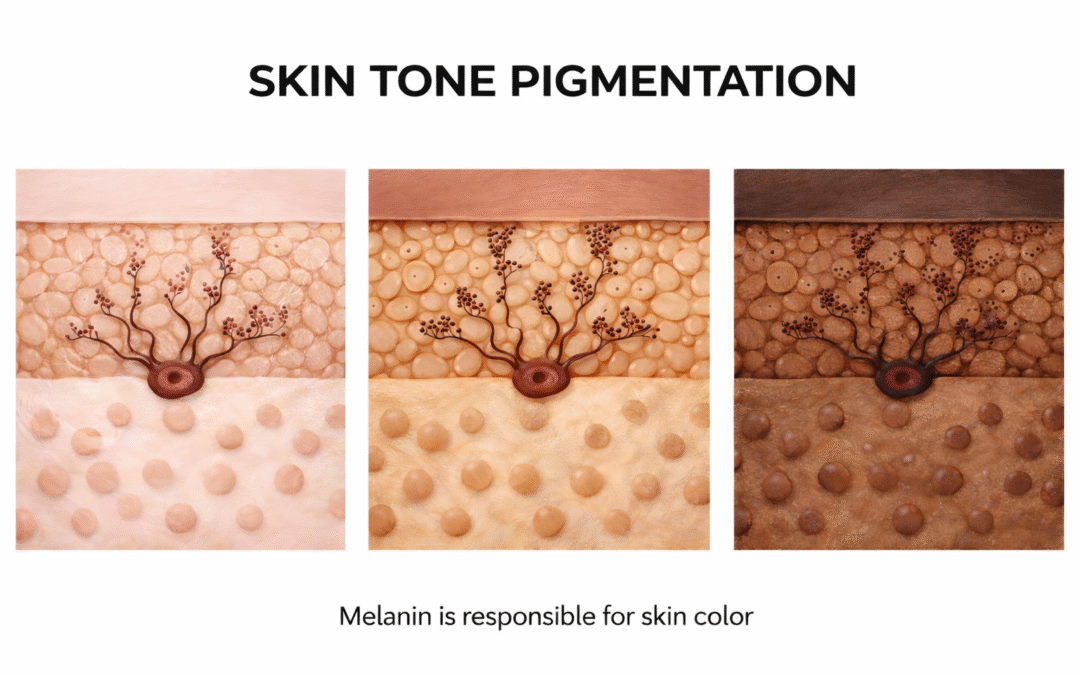
Melanin is synthesized by melanocytes and transferred to surrounding keratinocytes via melanosomes. Skin color is influenced not by melanocyte number but by:
- Melanocyte activity
- Melanosome size and distribution
- Rate of melanin degradation
Disruption at any level can result in hyperpigmentation.
Classification of Pigmentation Disorders
- Epidermal Pigmentation
- Increased melanin within the epidermis
- Appears light to dark brown
- Enhances under Wood’s lamp
Examples:
- Solar lentigines
- Ephelides
- Early post-inflammatory pigmentation
- Dermal Pigmentation
- Melanin deposited within dermal macrophages
- Appears bluish-grey or slate brown
- No enhancement under Wood’s lamp
Examples:
- Dermal melasma
- Drug-induced pigmentation
- Nevus of Ota
- Mixed Pigmentation
- Involves both epidermal and dermal components
- Most common and most challenging form
Examples:
- Melasma (majority of cases)
- Post-Inflammatory Hyperpigmentation (PIH)
- Secondary to inflammation or injury
- Common in higher Fitzpatrick skin types
Triggers include:
- Acne
- Procedures
- Burns
- Inflammatory dermatoses
Pathophysiological Triggers in Pigmentation
Pigmentation is rarely a standalone melanocyte issue. Key contributors include:
- UV and visible light exposure
- Inflammatory mediators
- Hormonal influence
- Vascular component
- Impaired skin barrier
- Oxidative stress
This explains why monotherapy often fails in chronic pigmentation disorders.
Clinical Evaluation: A Crucial Step
Before initiating treatment, clinicians must assess:
- Depth of pigmentation
- Fitzpatrick skin type
- Duration and triggers
- Previous treatment history
- Risk of rebound or PIH
Correct diagnosis determines treatment safety and success.
In-Clinic Aesthetic Modalities for Pigmentation Management
- Chemical Peels
Superficial and medium-depth peels help by:
- Reducing epidermal melanin load
- Accelerating keratinocyte turnover
- Enhancing penetration of adjuvant therapies
Peels must be carefully selected to avoid inflammation-induced rebound pigmentation.
- Energy-Based Devices
Laser and light-based treatments target pigment chromophores and vascular components.
Key considerations:
- Proper wavelength selection
- Conservative parameters in darker skin types
- Combination with barrier repair protocols
Energy devices are adjunctive, not standalone solutions.
- Microneedling-Assisted Therapies
Microneedling improves pigmentation by:
- Modulating melanocyte activity
- Improving dermal remodeling
- Enhancing delivery of regenerative actives
- Reducing chronic inflammation
It is particularly useful in mixed and recalcitrant pigmentation.
- Injectable and Regenerative Approaches
Emerging regenerative treatments focus on:
- Reducing inflammation
- Improving dermal health
- Restoring normal melanocyte–keratinocyte communication
These approaches address the root biological dysfunction, not just melanin excess.
Combination Therapy: The Gold Standard
Current evidence supports multimodal treatment, combining:
- In-clinic procedures
- Barrier repair strategies
- Strict photoprotection
- Maintenance protocols
Pigmentation is a chronic condition and requires long-term management, not one-time correction.
The Role of Patient Education
Managing expectations is critical. Patients must understand:
- Pigmentation improves gradually
- Maintenance is essential
- Recurrence is possible without compliance
This improves outcomes and patient satisfaction.
Summary:
Pigmentation disorders demand a scientific, layered, and cautious approach. Successful treatment depends on:
- Accurate diagnosis
- Understanding depth and etiology
- Selecting appropriate in-clinic modalities
- Avoiding aggressive, one-size-fits-all treatments
In aesthetic dermatology, pigmentation management is not about bleaching the skin—it is about restoring biological balance and skin health.